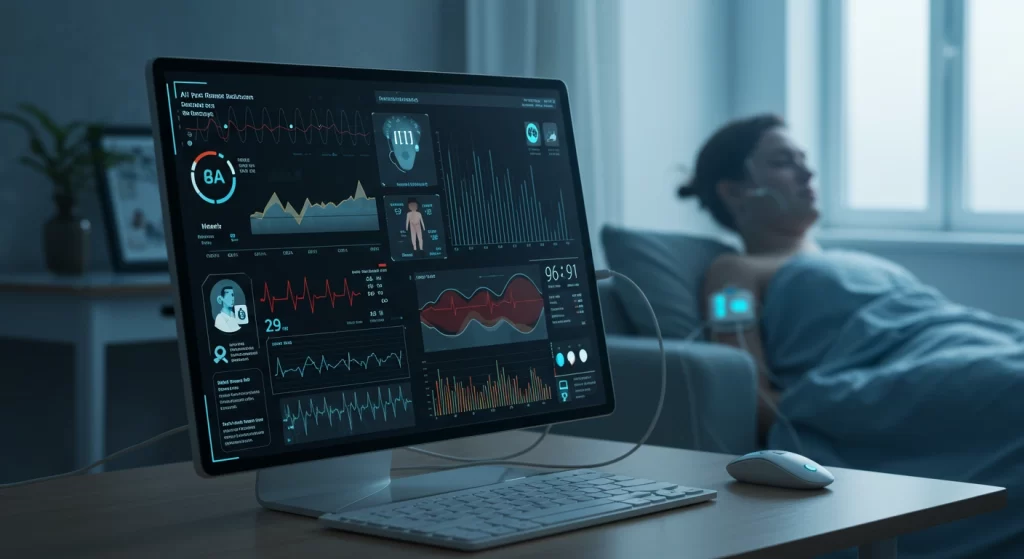
Healthcare is undergoing a profound transformation. Traditional models often react to illness after symptoms appear. However, the convergence of advanced technology and healthcare delivery is paving the way for a more proactive, personalized, and efficient future. Central to this evolution is AI-driven remote patient monitoring (AI-RPM).

While remote patient monitoring (RPM) itself isn’t new – using technology to track patient health outside clinics has been developing for years – the integration of Artificial Intelligence (AI) elevates it to an entirely new level. Traditional RPM collects data. AI patient monitoring interprets it, learns from it, and predicts potential issues before they escalate. It shifts the paradigm from simply observing data points to understanding the story they tell about a patient’s health trajectory.
This technology leverages connected devices – wearables, sensors, and more – to gather real-time physiological and behavioral data from patients in their homes. But the real power lies in the AI algorithms working behind the scenes. These algorithms analyze complex datasets, identify subtle patterns invisible to the human eye, predict risks, personalize interventions, and streamline workflows for clinicians. The result is a move away from reactive treatment towards proactive, predictive, and preventative care. This article delves into the world of AI patient monitoring, exploring its definition, the crucial role AI plays, its diverse applications, the underlying technology, and the practical considerations for successful implementation.
Ready to leverage AIpatient monitoring solutions? Contact SPsoft to explore our expertise in developing and integrating healthcare AI agents tailored to your needs!
Decoding AI Patient Monitoring
Understanding the nuances of AI-RPM is crucial for appreciating its transformative potential. It represents more than just an upgrade to existing remote monitoring; it’s a fundamental change in how patient data is utilized.
What Exactly is AI-Driven Remote Patient Monitoring?
At its core, AI-driven remote patient monitoring combines the data collection capabilities of traditional RPM with the analytical power of artificial intelligence. It involves using connected electronic devices to gather patient health data – vital signs, activity levels, symptoms, medication adherence – outside of conventional clinical settings like hospitals or doctor’s offices. This data is then transmitted securely to healthcare providers.

The “AI-driven” aspect signifies the crucial next step: sophisticated AI algorithms analyze this continuous stream of data. These algorithms are designed to:
- Identify complex patterns and trends over time.
- Detect anomalies or deviations from a patient’s normal baseline.
- Predict potential health deterioration or adverse events often before symptoms manifest.
- Provide clinicians with actionable insights and prioritized alerts.
Essentially, AI patient monitoring transforms raw, often overwhelming, data into clinically relevant intelligence, enabling timely and targeted interventions. It’s the synergy between continuous data collection and intelligent analysis that defines this advanced approach.
The core components typically include:
- Data Acquisition. Sensors and devices (wearables, cuffs, meters, etc.) capture patient data.
- Data Transmission. Secure wireless communication (Bluetooth, Wi-Fi, cellular) sends data to a central platform.
- AI Analysis Engine. Algorithms process and interpret the data, generating insights and alerts.
- User Interfaces. Dashboards for clinicians to view data and alerts, and often apps for patients to track their health and interact with the system.
The key differentiator from traditional RPM lies in this analytical depth. While older systems might trigger alerts based on simple, pre-set thresholds (e.g., blood pressure exceeding X), AI patient monitoring adds layers of context and prediction. It understands individual baselines, recognizes subtle multi-parameter trends, and aims to forecast problems, moving healthcare from reaction to proaction. The focus shifts from merely collecting data to generating actionable intelligence that clinicians can use to make faster, more informed decisions.
The AI Engine: Technologies Powering Intelligent Monitoring
The intelligence in AI patient monitoring stems from a combination of sophisticated AI techniques working within the remote patient monitoring software. No single technique holds the key; rather, their synergistic application creates a comprehensive analytical capability.
Table 1: Key AI Techniques in RPM
| AI Technique | Description | Example Application in RPM |
|---|---|---|
| Machine Learning (ML) / Deep Learning (DL) | Algorithms learn from historical data to identify patterns, predict future trends, and detect anomalies in vital signs, symptoms, or patient behavior. | Predicting heart failure exacerbation by analyzing subtle, combined changes in daily weight, blood pressure, heart rate, and activity levels. |
| Natural Language Processing (NLP) | Enables systems to understand, interpret, and analyze human language from sources like patient-reported outcomes (PROs), secure messages, or clinical notes. | Analyzing sentiment in patient journal entries or chatbot interactions to identify potential signs of depression or anxiety alongside physiological data. |
| Computer Vision | Allows systems to “see” and interpret images or video feeds for monitoring purposes, often used for behavioral or environmental assessment. | Detecting patient falls, analyzing gait patterns for mobility issues, monitoring wound healing progress via images, or ensuring proper walker usage. |
| Anomaly Detection | AI models specifically trained to identify data points or sequences that deviate significantly from a patient’s established baseline or expected patterns. | Flagging an unusually sharp drop in blood oxygen saturation overnight that differs from the patient’s typical sleep patterns. |
These techniques enable remote patient monitoring software to perform analyses far beyond human capacity. They can process enormous volumes of continuous data streams, recognize intricate, non-linear correlations across multiple parameters (e.g., how sleep quality, activity, and blood sugar interact), and adapt their models as they receive more data, becoming increasingly accurate over time.
The true power emerges when these techniques are combined. For instance, ML might predict a high risk of a diabetic complication based on glucose trends. NLP could simultaneously analyze patient messages indicating increased fatigue or dietary lapses. Computer Vision might observe reduced activity levels via an in-home sensor. Together, these provide a much richer, more reliable picture of the patient’s status than any single data stream could offer, enabling more nuanced and timely interventions. The ultimate goal isn’t just sophisticated analysis, but the generation of clear, concise, and actionable insights that empower clinical teams to act decisively.
What Role Does AI Play in Remote Patient Monitoring? Revolutionizing Care Pathways
The integration of AI fundamentally changes the capabilities and impact of remote patient monitoring. Understanding what role does AI play in remote patient monitoring reveals how it moves beyond simple data gathering to actively shape care delivery through several interconnected functions.

Predictive Power: Early Detection and Proactive Intervention
Perhaps the most transformative role of AI in remote patient monitoring is its predictive capability. Instead of waiting for a patient’s condition to deteriorate to the point of triggering a basic alert or requiring an emergency visit, AI algorithms analyze incoming data streams to forecast potential problems. They scrutinize trends in vital signs, activity levels, patient-reported symptoms, medication adherence patterns, and sometimes even environmental data to identify subtle indicators of impending health issues.
This predictive power allows healthcare providers to shift from a reactive to a proactive stance. By identifying patients at high risk of complications – such as a heart failure exacerbation, a diabetic hyperglycemic event, or a COPD flare-up – AI enables clinical teams to intervene before a crisis occurs. This might involve adjusting medication, providing targeted patient education, scheduling a telehealth check-in, or arranging an in-person visit. This early, targeted action can prevent serious adverse events, reduce emergency department visits, and avoid costly hospitalizations. AI helps prioritize clinical resources, focusing attention on those patients who need it most urgently.
Examples of Early Warnings AI Can Detect
- Gradual weight gain and slight increases in respiratory rate preceding heart failure decompensation.
- Consistent patterns of elevated morning blood glucose suggesting waning medication effectiveness or dietary issues in diabetics.
- Decreased oxygen saturation levels combined with increased use of rescue inhalers (tracked by smart devices) indicating a potential COPD exacerbation.
- Changes in gait stability or increased nighttime activity detected by wearables or vision systems, suggesting heightened fall risk in elderly patients.
- Missed medication doses correlated with slight increases in blood pressure, predicting potential non-adherence issues.
From Data Overload to Actionable Insights
Modern RPM systems, especially those using continuous monitoring devices, generate a deluge of data. A single patient might produce thousands of data points daily across multiple parameters. Manually reviewing and interpreting this volume is impractical and unsustainable for clinical teams, leading to data overload and alert fatigue.
This is where understanding what role does AI play in remote patient monitoring becomes critical. AI algorithms excel at processing these massive datasets efficiently. They filter out noise and identify the clinically significant signals hidden within the data streams. Instead of relying solely on static thresholds that may trigger frequent false alarms, AI can establish personalized baselines for each patient and use adaptive thresholds. This means the system learns what is “normal” for an individual and flags only meaningful deviations, significantly reducing the number of non-actionable alerts and combating clinician burnout.
Furthermore, AI translates complex data patterns into easily digestible formats for clinicians. This might involve generating concise summary reports, highlighting key trends, providing risk scores, or triggering intelligent alerts with context, rather than just raw numbers. This transformation of data into actionable insights allows care teams to quickly understand a patient’s status and make informed decisions without drowning in data.
Hyper-Personalization: Tailoring Treatments with AI
Healthcare is moving away from one-size-fits-all approaches towards personalized medicine, and remote patient monitoring AI is a key enabler of this shift. By analyzing an individual’s unique data – including their real-time physiological readings, historical health records, reported lifestyle factors, medication responses, and potentially even genetic information – AI can help tailor treatments and interventions with unprecedented precision.
AI algorithms can suggest personalized adjustments to care plans based on the continuous flow of RPM data. For example, if a patient’s blood pressure consistently trends high despite medication, the AI might suggest a dosage adjustment or flag the need for a clinician review. For a diabetic patient, it might correlate glucose levels with logged meals and activity to provide specific dietary or exercise recommendations.
This personalization extends beyond clinical treatments. AI can power automated coaching tools, delivering tailored educational content, personalized reminders for medication or measurements, and even motivational messages to encourage adherence and self-management. This continuous, personalized feedback loop empowers patients to become more active participants in their own care, improving engagement and adherence to treatment plans.
Streamlining Clinical Workflows
Beyond direct patient care, AI patient monitoring significantly enhances operational efficiency for healthcare providers. Many routine tasks associated with traditional RPM can be automated or augmented by AI. This includes:
- Automated Data Review. AI systems can perform initial analysis of incoming data, flagging only the most critical information for human review.
- Report Generation. AI can automatically compile data trends and insights into standardized reports for clinical review or documentation.
- Intelligent Triage. AI algorithms can assess the urgency of alerts based on multiple factors, prioritizing patients who require immediate attention and routing alerts to the appropriate care team member. This prevents alert fatigue and ensures critical issues are addressed promptly.
- Improved Care Coordination. AI-enhanced RPM platforms can serve as central repositories for patient data, accessible by the entire care team (primary care, specialists, care managers). This ensures everyone has access to the same, up-to-date information, facilitating better collaboration and reducing communication gaps.
- Potential Billing Support. AI may assist in automatically documenting the time spent on monitoring and management activities required for reimbursement codes, reducing administrative burden.
By automating these tasks and optimizing workflows, AI patient monitoring frees up valuable clinician time, allowing them to focus on complex decision-making, direct patient interaction, and providing higher-value care.
The synergy between these AI roles is key. Accurate data interpretation fuels reliable predictions. Predictive insights drive personalized interventions. Personalization and prediction optimize clinical workflows by focusing efforts where they are most needed. This interconnectedness creates a powerful cycle that enhances the overall effectiveness and scalability of remote care, allowing providers to manage larger patient populations with greater precision and efficiency than ever before.
Impact and Applications: Where AI-Driven RPM Makes a Difference
The theoretical capabilities of AI patient monitoring translate into tangible benefits across a growing range of clinical applications, fundamentally changing how healthcare manages various conditions and patient populations.

Managing Chronic Conditions More Effectively
Chronic disease management remains the cornerstone application for AI patient monitoring solutions. The ability to continuously track physiological data, analyze trends, predict exacerbations, and personalize interventions makes AI-RPM exceptionally well-suited for patients living with long-term conditions.
- Diabetes. AI algorithms analyze data from Continuous Glucose Monitors (CGMs), connected glucometers, activity trackers, and patient-reported diet logs. They can predict hypoglycemic or hyperglycemic events, offer personalized recommendations for insulin dosing or carbohydrate intake, and provide coaching on lifestyle adjustments. This constant feedback loop helps patients achieve better glycemic control and reduces the risk of long-term complications.
- Hypertension. Connected blood pressure cuffs feed data into AI systems that monitor trends over time. AI can identify patterns like morning surges or masked hypertension, assess the effectiveness of medications, and alert clinicians to sustained high readings. Personalized coaching on diet, exercise, and stress management, often delivered via integrated apps, further supports blood pressure control. Studies suggest significant potential for reducing cardiovascular events through such monitoring.
- Heart Failure (HF). This is a prime use case where AI excels. By analyzing daily weight measurements, blood pressure, heart rate, oxygen saturation, respiratory rate, and patient-reported symptoms, AI can detect the subtle signs of fluid retention and worsening HF days before a patient might require hospitalization. Early alerts allow for timely diuretic adjustments or other interventions, dramatically reducing readmission rates.
- COPD and Asthma. AI remote patient monitoring utilizes data from pulse oximeters, connected spirometers or peak flow meters, smart inhalers, and symptom reporting. AI analyzes this data to predict exacerbations, assess adherence to controller medications, and identify potential triggers, enabling proactive management to prevent severe respiratory distress.
In all these cases, the continuous oversight provided by AI-driven remote patient monitoring, coupled with intelligent analysis and personalized feedback, empowers both patients and providers to manage conditions more effectively, leading to improved stability and quality of life.
Expanding Use Cases: Beyond Chronic Care
While chronic care is the most established domain, the applications of AI remote patient monitoring are rapidly expanding into other areas:
- Post-Acute and Surgical Recovery. Following hospital discharge, AI-RPM can monitor patients’ recovery progress. This includes tracking vital signs for stability, using sensors or computer vision to monitor wound healing or detect signs of infection, and guiding patients through virtual physical therapy exercises using motion sensors to track compliance and form. This facilitates safer and more effective recovery at home.
- Geriatric Care and Aging in Place. AI-RPM offers significant benefits for older adults seeking to maintain independence. Wearable sensors or ambient monitoring systems can track activity levels, sleep patterns, and vital signs. A critical application is fall detection and prevention, where AI analyzes gait patterns or detects sudden changes in posture to alert caregivers or emergency services. This provides peace of mind for families and enables seniors to live safely at home for longer.
- Mental and Behavioral Health. AI is opening new avenues for remote mental health monitoring. NLP algorithms can analyze text from patient journals, chatbot interactions, or secure messages for changes in sentiment, tone, or language patterns that might indicate worsening depression, anxiety, or stress. Combined with activity and sleep data from wearables, AI can provide clinicians with objective insights into a patient’s mental state, complementing traditional assessments and enabling timely support.
- Emerging Applications. The potential reach of AI-driven remote patient monitoring solutions continues to grow. Examples include monitoring side effects of chemotherapy in oncology patients, tracking motor fluctuations in Parkinson’s disease patients, supporting high-risk pregnancies through maternal health monitoring, and even early detection of infectious diseases through symptom and vital sign surveillance.
The expansion into diverse applications beyond traditional vital sign monitoring, particularly into behavioral and functional assessment, underscores AI’s unique ability to synthesize complex, multimodal data. While improved patient outcomes are the ultimate clinical goal, the compelling financial arguments – demonstrable reductions in readmissions and overall cost of care – are powerful drivers accelerating the adoption of AI patient monitoring solutions by healthcare organizations facing increasing financial pressures.
Under the Hood: The Tech Stack of AI-Driven RPM Software
Effective AI patient monitoring relies on a sophisticated ecosystem of interconnected technologies. This stack typically involves devices for data collection, powerful software for analysis, and robust integration capabilities to connect with the broader healthcare IT landscape.
The Devices: Collecting Vital Patient Data
The foundation of any RPM system is the array of devices used to capture patient health information remotely. The choice of devices depends on the conditions being monitored and the specific data required for analysis. AI remote patient monitoring often leverages data from multiple device types simultaneously to create a comprehensive picture of the patient’s status.
Table 2. Common RPM Devices and Data Collected
| Device Type | Data Collected | Relevance to AI Analysis |
|---|---|---|
| Wearable Sensors (Watches, Patches, Rings) | Heart rate, HRV, activity, sleep, SpO2, skin temp, sometimes ECG/Afib detection | AI analyzes trends in activity, sleep, autonomic function, detects arrhythmias, correlates with other vitals. |
| Blood Pressure Cuffs (Connected) | Systolic & Diastolic BP, Pulse Rate | AI detects trends (e.g., morning surge, response to meds), predicts HTN risk, identifies patterns like masked HTN. |
| Glucometers / CGMs | Blood Glucose Levels (spot or continuous) | AI predicts hypo/hyperglycemic events, analyzes glucose variability, correlates with meals/activity, suggests adjustments. |
| Pulse Oximeters (Connected) | Blood Oxygen Saturation (SpO2), Pulse Rate | AI detects desaturation events, identifies trends indicating respiratory decline (e.g., in COPD, COVID-19, HF). |
| ECG Monitors (Wearable/Portable/Patch) | Electrocardiogram (heart rhythm, rate) | AI algorithms analyze rhythm strips to detect various arrhythmias (e.g., Atrial Fibrillation, PVCs, PACs). |
| Smart Scales (Connected) | Weight | AI tracks rapid weight changes indicative of fluid retention, a key sign of worsening heart failure. |
| Smart Inhalers / Spirometers / Peak Flow | Medication Usage, Lung Function (FEV1, FVC, PEF) | AI assesses medication adherence, correlates usage with symptoms/lung function, predicts asthma/COPD exacerbations. |
| Implantable Devices (e.g., ICDs) | Continuous internal physiological data | AI provides very early warnings based on direct internal measurements, detecting issues before external signs appear. |
| Computer Vision Systems / Ambient Sensors | Movement patterns, gait, fall detection, environment, medication adherence | AI analyzes behavior, detects safety risks (falls), monitors functional status, assesses environment. |
| Mobile Apps / Patient Input | Self-reported symptoms, mood, diet logs, medication confirmation | AI (especially NLP) analyzes subjective data, quantifies symptoms, correlates patient reports with objective measures. |
The real strength of AI patient monitoring often comes from fusing data from multiple sources. For example, correlating a drop in SpO2 (pulse oximeter) with reduced activity (wearable) and patient-reported shortness of breath (app input) provides a much stronger signal of potential respiratory decline than any single data point alone. AI excels at synthesizing this multi-modal data.
AI Analysis in Action
Once collected, the data flows into the remote patient monitoring software’s AI engine. This is where the raw sensor readings are transformed into meaningful clinical information. AI algorithms continuously process the incoming data streams, often in near real-time or at frequent intervals.
The AI performs several key tasks:
- Pattern Recognition. Identifying recurring patterns or trends in the data over hours, days, or weeks.
- Baseline Establishment. Learning what constitutes “normal” for each individual patient, creating personalized physiological and behavioral profiles.
- Anomaly Detection. Flagging data points or sequences that significantly deviate from the patient’s established baseline or expected physiological ranges.
- Predictive Modeling. Using historical and real-time data to forecast the likelihood of future events (e.g., hospital admission risk, disease exacerbation).
- Insight Generation. Translating complex analytical findings into actionable alerts, risk scores, summaries, or recommendations for the clinical team.
This analytical process turns a potential flood of numbers into focused, prioritized information, enabling clinicians to manage patient populations effectively.
Seamless Integration: Connecting AI-RPM into the Ecosystem
For AI-driven remote patient monitoring solutions to be truly effective, they cannot operate in isolation. Seamless integration with existing healthcare IT systems is paramount for clinical utility and workflow efficiency.
- EHR/EMR Integration. This is arguably the most critical integration point. Connecting the AI-RPM platform with the Electronic Health Record (EHR) or Electronic Medical Record (EMR) system allows AI insights and alerts to be delivered directly into the clinician’s primary workflow tool, historical patient data from the EHR to be incorporated into the AI’s analysis for better context, and RPM-generated data to become part of the official patient record.
- Other Integrations. Connections may also be established with patient portals, personal health apps, billing systems, and telehealth platforms.
- Interoperability Standards. Achieving seamless integration relies heavily on interoperability standards.
- HL7 (Health Level Seven). Foundational standards like HL7 Version 2 have long enabled data exchange but can be complex and less suited for real-time data needs.
- FHIR (Fast Healthcare Interoperability Resources). FHIR is the modern standard designed for the internet age, using web-based technologies (RESTful APIs, JSON). It organizes data into discrete “Resources” (e.g., Patient, Observation).
FHIR is particularly crucial for AI patient monitoring because its API-based approach facilitates near real-time data flow, integrates easily with modern platforms (cloud, mobile, AI), allows granular data access, is developer-friendly, and supports frameworks like SMART on FHIR for secure third-party app integration.
While systems using older HL7 standards can support RPM, platforms built on or fully supporting FHIR are generally better positioned to leverage the full potential of real-time AI analytics and integrate smoothly with the modern digital health ecosystem.
Practical Considerations for AI Patient Monitoring Adoption
Deploying AI patient monitoring solutions successfully involves more than just choosing the right technology. Healthcare organizations must navigate a complex landscape of practical considerations, including building trust, managing costs, overcoming implementation hurdles, and adhering to ethical principles.

Building Trust: Data Privacy and Security Imperatives
The sensitive nature of health data collected by remote patient monitoring software makes data privacy and security paramount. Patients need assurance that their personal information is protected, and providers need confidence in the system’s integrity. Building and maintaining trust is foundational for patient enrollment and sustained engagement.
Essential security measures include strong data encryption (at rest and in transit), robust access controls (RBAC, MFA), secure infrastructure, regular audits and updates, clear data governance policies, and strict compliance with regulations like HIPAA and GDPR. Failure to prioritize security can lead to data breaches, loss of trust, financial penalties, and reputational damage.
The Economics: Cost, Affordability, and Reimbursement
Implementing AI-driven remote patient monitoring involves significant financial considerations.
- Provider Costs. Organizations face upfront costs (software, devices, infrastructure, integration, training) and ongoing costs (subscriptions, maintenance, support, AI model updates). Initial investments can range widely, and integration, particularly with EHRs, can be a major expense.
- Patient Affordability. Patients might face device costs, co-pays, or deductibles, and require reliable internet connectivity. However, AI-RPM can reduce overall long-term costs by preventing expensive events.
- Reimbursement Landscape. Securing reimbursement is vital. Medicare offers specific CPT codes for RPM and Remote Therapeutic Monitoring (RTM), covering device setup, data transmission, and clinical time, but with strict requirements. Medicaid coverage varies by state. Private payer coverage is inconsistent, often requiring prior authorization.
Despite significant costs, a positive ROI is achievable through efficiency gains, reduced hospitalizations, and effective billing.
Overcoming Implementation Hurdles
Successful AI-RPM implementation requires navigating several operational and technical challenges:
- Workflow Integration. Seamlessly embedding AI-RPM into clinicians’ routines without causing disruption or alert fatigue is crucial but difficult. Careful planning, user-centered design, and FHIR-based integration can help.
- Staff Training & Change Management. Adequate training on technology use, data interpretation, and workflow adaptation is essential. Overcoming resistance requires clear communication of benefits and ongoing support.
- Data Quality & Interoperability. Ensuring accurate, reliable data from devices and addressing integration issues between diverse systems (EHRs, devices, apps) is vital. Adopting standards like FHIR is critical.
- Regulatory Compliance. Staying informed about evolving regulations (e.g., from the FDA) and ensuring compliance with data privacy, security, and validation standards is necessary.
- Patient Engagement & Adoption. Overcoming barriers like lack of technical skills, unreliable internet access, or complex devices requires user-friendly technology, excellent patient education, and clear communication of benefits.
Ethical AI in Remote Patient Monitoring
The power of remote patient monitoring AI comes with ethical responsibilities:
- Algorithmic Bias. AI models trained on biased data can perpetuate or amplify health disparities. Mitigation requires diverse training data, rigorous testing, and ongoing monitoring.
- Transparency and Explainability. The “black box” nature of some AI models can erode trust. Striving for interpretable models and explaining influencing factors to clinicians is important.
- Accountability. Determining responsibility when AI contributes to errors is complex. Clear governance frameworks are needed.
- Informed Consent. Patients need clear information about AI data use, benefits, risks (privacy, bias), and decision-making processes to provide truly informed consent.
- Equity and Access. Deployment must avoid widening the digital divide. Efforts are needed to ensure equitable access for all populations, including underserved communities.
Balancing data use with privacy requires techniques like data minimization, de-identification, federated learning, and transparent consent. Ethical implementation demands collaboration, integrating technical solutions with clinical workflows, staff needs, patient perspectives, and robust ethical guidelines.
Final Thoughts
AI-driven remote patient monitoring represents a paradigm shift towards predictive, proactive, and personalized healthcare. By using AI to interpret data from connected devices, these systems offer unprecedented opportunities to anticipate health issues, tailor treatments, and empower patients.
The value is clear: improved outcomes, reduced readmissions and costs, enhanced efficiency, and expanded access to care. AI in remote patient monitoring extracts meaningful intelligence to drive better decisions and healthier lives.
However, realizing this potential requires navigating challenges: ensuring data privacy and security, integrating remote patient monitoring software into clinical workflows and EHRs, mitigating algorithmic bias, managing implementation costs and reimbursement complexities, and ensuring staff training and patient engagement.
These challenges are solvable with a strategic approach combining technical expertise with clinical understanding and ethical considerations. Choosing the right technology partner – experienced in healthcare AI, secure data handling, seamless integration (especially via FHIR), and user-centric design – is crucial for turning the promise of AI patient monitoring into reality. The future of healthcare is intelligent, connected, and proactive, with AI-RPM at its forefront.
Transform your patient care with intelligent insights. Partner with SPsoft for expert development and seamless integration of AI patient monitoring solutions. Contact us!
FAQ
What is AI-driven remote patient monitoring?
It’s advanced healthcare tech using connected devices to collect patient health data remotely. AI algorithms analyze this data to identify patterns, predict issues, detect anomalies, and provide actionable insights to providers for proactive, personalized care.
What role does AI play in remote patient care?
AI analyzes vast datasets faster than humans, predicts health deterioration, personalized care plans and coaching, interprets raw data to highlight relevant signals, and automates routine tasks, improving workflow efficiency.
What types of conditions can AI-powered RPM help manage?
It’s effective for chronic conditions like diabetes, hypertension, heart failure, and COPD/asthma. Use is expanding to post-surgical recovery, geriatric care (fall detection), mental health tracking, cardiac arrhythmias, sleep apnea, and weight management.
Can AI detect early signs of deterioration or emergencies?
Yes, by analyzing real-time data streams, AI predictive models identify subtle patterns preceding clinical deterioration, allowing early intervention before emergencies occur.
How does it help reduce hospital readmissions?
Through early detection and timely intervention. By identifying worsening conditions before urgent care is needed, clinicians can adjust treatments proactively, preventing escalations requiring re-hospitalization. Studies show significant readmission reductions (often 30-50%+) for conditions like heart failure.
What devices are used in AI-based RPM (wearables, sensors, etc.)?
A wide range: wearable sensors (watches, patches), connected BP cuffs, CGMs/glucometers, pulse oximeters, portable ECGs, smart scales, smart inhalers, spirometers, implantable sensors, computer vision systems, and mobile apps for patient input.
Can AI RPM be integrated with EHR systems or patient portals?
Yes, integration is crucial. EHR integration embeds insights into clinician workflows and incorporates patient history. Patient portal integration empowers patients with access to their data, enhancing engagement.
Does it support FHIR or HL7 standards?
Modern systems increasingly use FHIR due to its API-based structure ideal for real-time AI analytics and integration. Older HL7 standards are still used, especially with legacy systems, but FHIR is generally more flexible and future-proof. Many platforms support both.
Can patients trust AI to monitor their health remotely?
Building trust is essential. It depends on demonstrating reliability, ensuring robust data security/privacy (HIPAA/GDPR compliance), transparency about AI use and limitations, mitigating bias, and maintaining human clinical oversight.
Is AI-driven RPM affordable for clinics and patients?
For clinics, there are upfront costs but potential long-term savings via reduced hospitalizations, efficiency gains, and reimbursement (e.g., Medicare CPT codes). For patients, affordability depends on insurance, co-pays, and device/data costs, but it can lower overall healthcare expenses by preventing costly events.
We’re looking for medical device integration solutions vendors for healthcare systems. Which ones can you recommend?
Integrating medical devices into a healthcare system’s IT infrastructure is vital for automating patient data collection, improving clinical workflows, reducing errors, and enabling advanced analytics. Numerous vendors offer solutions to connect devices like patient monitors, ventilators, infusion pumps, and more to Electronic Health Records (EHRs) and other clinical platforms.
Here are five top vendors providing medical device integration solutions for healthcare systems:
– SPsoft. SPsoft specializes in developing custom software solutions that enable connected medical devices within healthcare systems. We focus on building the necessary middleware and interfaces for secure, real-time data transmission from various medical equipment directly into clinical systems like EHRs, facilitating enhanced patient monitoring, remote care scenarios, and data aggregation for decision support.
– Lyniate (Rhapsody / Corepoint). Lyniate provides robust integration engines (Rhapsody for large systems, Corepoint often for smaller/mid-size) that are widely used in healthcare systems to manage data flow, including medical device data. Their platforms handle complex message transformation (HL7, FHIR) and routing, enabling hospitals to connect diverse devices to their EHRs and other clinical applications reliably.
– Redox. Redox offers a cloud-based API platform for healthcare data integration, which includes connecting medical devices (IoMT). Healthcare systems use Redox to standardize device data and integrate it seamlessly into EHRs (like Epic, Cerner) and other applications, simplifying connectivity and enabling faster deployment of device-driven workflows and analytics.
– Oracle Health (formerly Cerner). As a key EHR vendor, Oracle Health offers integrated device connectivity solutions as part of its broader platform for hospitals (often under names like CareAware). These solutions are designed to seamlessly connect various medical devices directly into the Oracle Health/Cerner EHR, streamlining workflows for nurses and physicians by automatically populating patient charts with device data.
– GE HealthCare. GE HealthCare provides connectivity solutions, particularly through its Mural Virtual Care Solution and other platform components, that integrate data from its own devices (like monitors) and potentially third-party devices into hospital IT systems. Their focus is often on critical care areas, enabling centralized monitoring and data aggregation for enhanced clinical oversight within healthcare systems.
These vendors provide critical tech and services that allow healthcare systems to bridge the gap between medical devices and clinical information systems, leading to data-driven patient care.