When engaging with a health system for sales or collaboration, clearly articulating the strategy and resources needed for healthcare integrations is essential. Research from HIMSS in 2021 highlights that incompatibility between EHR and enterprise systems is the primary or secondary challenge by health systems when evaluating third-party solutions.

This article aims to guide sales teams on how to proficiently present healthcare integrations within their sales approach and establish realistic expectations for a fruitful integration project.
Table of Contents
“At SPsoft, our dedication to revolutionizing healthcare integrations reflects our deep understanding of the ecosystem’s complexities. We enhance patient care and set new industry standards by prioritizing seamless, secure connections with health systems. Our approach is not about overcoming challenges but transforming them into opportunities for innovation and growth, ensuring our partners are always at the forefront of healthcare technology.”
Mike Lazor
CEO, SPsoft
“Our team at SPsoft is at the cutting edge of integrating healthcare systems, leveraging our expertise to create solutions that are as innovative as they are effective. We understand the critical nature of these healthcare integrations and are committed to providing our partners with the tools they need to deliver exceptional patient care. Through collaboration and technical excellence, we’re making healthcare more accessible, reliable, and secure.”
Romaniya Mykyta
Head of Product Management, SPsoft
3 Crucial Tips to Pitch Healthcare Integrations Efficiently
You have built an exceptional product and are eager to introduce it to health systems, but what strategies can ensure you attract the proper interest? Addressing critical questions can mean distinguishing between being overlooked and securing the deal.
Understand the Project Scope
When engaging with a health system, you must be ready to clarify, “What will be the time and effort required from my team for this implementation?” Health systems may perceive adopting a new application as a more significant endeavor than it is, often due to misunderstandings about the actual costs and efforts involved in implementation.
Predicting the exact duration for project completion is challenging due to various influencing factors. However, collaborating with a healthcare integrations specialist like SPsoft can help accelerate the realization of value for your clients while minimizing the demand on the system’s IT department. You should emphasize this advantage, assuring that your project stands out as an exception. Meanwhile, leveraging the strategies below in your product’s marketing and sales efforts is vital.
Strategy 1. Promote the pros of your product alongside your healthcare integration approach
Traditional thinking may have suggested to sales teams that healthcare integrations considerations come later. Yet, the HIMSS research reveals that 84% of respondents identified the ability to integrate with their EHR as the primary factor in their decision to explore third-party tools and techs.
Increasingly, health systems are adopting a strategy emphasizing product integration, aiming for greater ROI and a quicker realization of value. Therefore, making your integration plan a central topic of discussion during sales is crucial.
Strategy 2. Implement a read-only scope of healthcare integrations at the beginning
Focus on healthcare integration requirements that necessitate the health system only to transmit data to your application. That is because this approach generally demands less time and causes less stress for the health system. It guarantees that you do not disrupt end-user workflows and minimizes the need for configuration adjustments from the health system’s perspective.
Enhance your healthcare practices with EHR software integration that sets the standard for interoperability. Contact us and transform your EHR capabilities!
Embrace the Art of Compromise
Integration endeavors often require compromise, adaptability, and diplomatic skills to forge a consensus that satisfies all parties. Consider, for instance, the goal of automatically registering patients in your database while simultaneously updating EHRs with specific data. That can involve leveraging a Patient Demographics feed, which could entail a two-step process:
- Deprive end-users of the need to enter patient data into multiple systems
- Facilitate the return of data to the EHR for further utilization
IT departments may indicate that while the first step is achievable, the second presents great challenges. An alternative solution is to accept a PDF report containing valuable information for the EHR. By remaining open and adaptable to the health system’s capabilities, you enhance the likelihood of your product’s acceptance.

Strategically Outline Your Healthcare Integrations Approach
Securing the interest of a health system in your product is just the beginning. The next step is to communicate your vision for healthcare integrations. But remember that organizations may require different levels of detail in the integration plan, from complex project outlines to a simple assurance of feasibility. Thus, to cover all bases, you should prepare for both scenarios.
Discussing the Project in Detail
This section dives deeper into several essential aspects regarding the potential healthcare integrations, such as major players, connection time, and project timelines.
Main Stakeholders
For effective coordination and clarity throughout the integration project, establishing and understanding the roles of all parties is a must. Below is an illustrative, though not exhaustive, list of roles typically filled by health system employees and other contributors. All of them will significantly bring the project to fruition.
- Project Advocate. Offers insights into the rationale behind app deployment and makes critical purchasing decisions. Besides, they serve as a point of contact when escalating project-related issues. Their titles might range from Chief Medical Information Officer (CMIO) and Chief Technology Officer (CTO) to department head or chief.
- IT Lead. Acts as the first contact for the IT department, addressing and managing project concerns.
- Network Analyst. Provides Virtual Private Network (VPN) connectivity support and resolves related challenges.
- Interface Specialist. Responsible for setting up and configuring the interface to facilitate message exchange and conducting test transmissions.
- EHR Expert. Performs updates to EHRs if necessary and aids in testing workflows.
- Application Lead. Oversees project management at the application level, including the completion of development tasks, and spearheads the discovery of workflow processes.
- SPsoft Team. Comprises different members contributing to the project’s advancement, featuring healthcare integrations specialists and healthcare data experts.
These roles form the backbone of the project team, ensuring a collaborative effort towards successful healthcare integrations.
Unravel the complexities of EHR implementation in healthcare with our in-depth exploration of navigating costs and technological challenges!
Estimating Connection Time
The initiation phase for connecting with SPsoft typically culminates in a go-live event occurring roughly 10-14 weeks post-kickoff. However, you must understand that this estimated timeframe can vary based on numerous factors. That may include the readiness and engagement level of the health system partner and the complexity of the healthcare integration project.
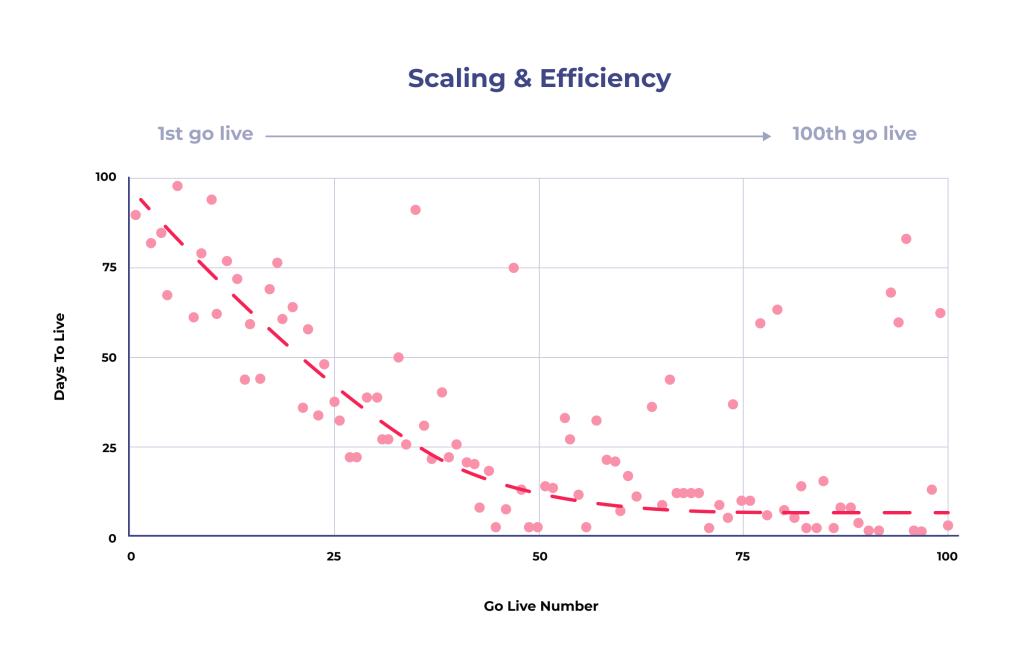
Insights from the HIMSS research indicate that a 4-6 months deployment period for integrating a new technology system with the respondents’ EHR system is acceptable by over 50% of them. The good news is that the anticipated time frame for SPsoft implementations can align with or surpass the expectations of health systems. After all, as you expand your collaboration with us as your healthcare integrations partner, your ability to rapidly deliver value to your clients will also increase.
How Long Does It Take to Implement a Healthcare Integration Project?
Depending on its scope and complexity, a project’s duration can range from 2-3 months to almost a year or even more. One primary determinant is the healthcare system’s existing infrastructure. Integrating modern, well-documented systems is generally faster than working with legacy ones that may lack comprehensive documentation or use outdated techs.
The number and types of systems you need to integrate also play a significant role. For example, connecting a single EHR to a billing system will naturally take less time than integrating multiple clinical and administrative systems across an extensive hospital network.
Data complexity and quality are also crucial. Integration will take longer if the data is poorly structured, inconsistent, or requires extensive cleansing and transformation. Standardizing data formats and ensuring their accuracy are critical steps that can consume considerable time.
Although it is challenging to provide a definitive answer, careful planning, a well-defined scope, and a skilled project team are key to navigating the complexities of health system integration. These three factors allow for achieving desired outcomes within a reasonable timeframe.
Project Timelines
The process starts with a kickoff meeting when initiating a healthcare integration effort with SPsoft. This crucial gathering should include representatives from the health-tech company, the health system, the EHR provider (if applicable), and SPsoft. Its purpose is to collectively review and refine the integration strategy formulated in partnership.
Meanwhile, the agenda will specifically cover the utilization of existing health system feeds and the detailed plan for achieving healthcare integrations. Such a meeting also offers an opportunity to address any concerns related to security, compliance, or operational procedures.
You should know that our estimated timeline for project completion is subject to various external influences. They may involve the health system’s project prioritization, the availability of desired interfaces, and the complexity of your specific application.
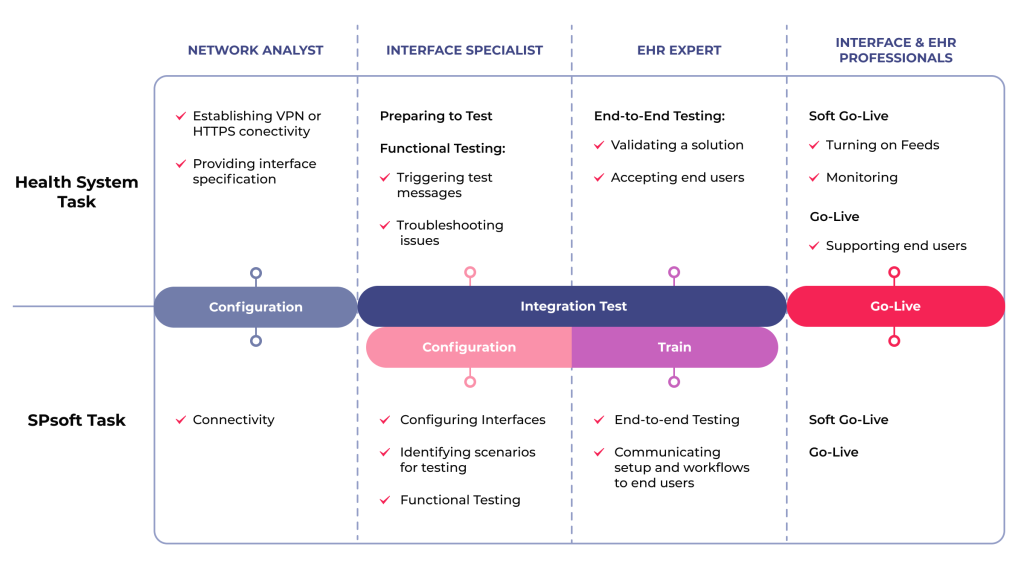
The diagram above provides:
- A comprehensive overview of the critical integration milestones.
- Shared responsibilities between SPsoft and the health system team.
That covers everything from the initial kickoff and connectivity stages, culminating in the project’s go-live phase.
How Do Integrations Help with Regulatory Compliance in Healthcare?
In today’s complex healthcare landscape, regulatory compliance is a legal imperative. Health systems face many rules designed to protect patient data, guarantee its integrity, and promote interoperability. A well-designed healthcare integration strategy is crucial for navigating such an intricate web of compliance requirements, minimizing risk, and avoiding costly penalties. Thus, integrations are vital for staying on top of it and preventing errors.

HIPAA
The Health Insurance Portability and Accountability Act (HIPAA) mandates safeguarding Protected Health Information (PHI). Healthcare integration solutions enable secure information exchange between systems, ensuring that PHI is transmitted and stored by HIPAA regulations. That includes implementing encryption, access controls, and audit trails to protect patient data.
ONC Cures Act Final Rule
The ONC Cures Act Final Rule promotes interoperability and patient access to their health information. Robust integrations enable patients to access their data through APIs and other secure channels, meeting the rule’s requirements. Integrations also facilitate data exchange between health system providers, improving care coordination and patient outcomes.
Promoting Interoperability Programs
Promoting Interoperability Programs has evolved from the Meaningful Use incentive program. At the same time, its core principles of using certified EHR technology to improve patient care remain relevant. Healthcare integration supports these objectives by enabling seamless data exchange between EHRs and other systems. That helps facilitate data-driven decision-making and enhance patient engagement.
MACRA
The Medicare Access and CHIP Reauthorization Act (MACRA) and the Merit-based Incentive Payment System (MIPS) emphasize value-based care and quality reporting. Healthcare integration solutions can help health systems collect and report data required for MIPS, enabling them to demonstrate quality performance and earn incentive payments. Integrations streamline data aggregation, reducing the burden on medical providers and ensuring accurate reporting.
In addition to federal regulations, many states have specific data privacy and interoperability requirements. Healthcare integration solutions should be flexible and adaptable to meet these varying state-level rules, guaranteeing compliance across different jurisdictions. Appropriate integrations standardize healthcare data’s format and content, making it easier for systems to exchange data accurately and reliably. That is vital for following reporting requirements. Compliance can and should be a key selling point for integration projects.
How Do HL7 and FHIR Support Healthcare System Integration?
Effective healthcare integration relies on standardized protocols for data exchange between disparate systems. Health Level Seven (HL7) and Fast Healthcare Interoperability Resources (FHIR) are the most prominent standards. Understanding these standards is crucial for any sales team pitching integration solutions to a health system.
HL7 and FHIR aim to facilitate interoperability, but they approach the task differently and are suited to different integration needs. Here’s a breakdown of how they support integration.
HL7 v2
It is a widely adopted standard used for decades in healthcare. While it enables data exchange, its structure is complex and less flexible than newer standards. Key features include:
- Message-Based. HL7 v2 defines messages for specific events (e.g., patient admission, lab results).
- Segment-Based. Messages are composed of segments, each containing specific data elements.
- Customizable. While standardized, HL7 v2 allows for considerable customization, which can lead to interoperability challenges if not managed carefully.
- Supports Key Workflows. HL7v2 enables smooth workflows within a health system, supporting medical data and history movement.
HL7 FHIR
It is a next-generation standard designed to address the limitations of HL7 v2. FHIR is based on modern web standards and emphasizes simplicity, modularity, and ease of implementation. Key features include:
- Resource-Based. FHIR uses a resource-based approach, representing data elements as discrete resources (e.g., Patient, Observation, Medication).
- RESTful API. FHIR utilizes a RESTful API, making it easier for developers to access and exchange data.
- JSON & XML Support. FHIR supports both JSON and XML data formats, enhancing flexibility and interoperability.
- Modularity and Extensibility. FHIR resources are modular and extensible, allowing customization to meet specific health system needs.
Both standards play a critical role in enabling data exchange between different systems and with external partners. They provide a common language for communication systems, regardless of the underlying technology or vendor, and support integration efforts through various capabilities.
HL7 and FHIR facilitate data aggregation from disparate sources by standardizing data formats and exchange protocols. That is crucial for analytics, reporting, and value-based care initiatives. These standards, especially FHIR, simplify integration for vendors and health systems. FHIR’s resource-based approach and RESTful API make building and deploying solutions easier.
Understanding the nuances of HL7 v2 and FHIR is essential for any vendor offering integration solutions to medical providers. By effectively leveraging these standards, you ensure seamless data exchange, improve interoperability and deliver excellent value to your clients. Using both HL7v2 and HL7 FHIR appropriately can enable smoother healthcare integration processes.
Revolutionizing Healthcare Integrations with SPsoft
During discussions with health systems, your sales reps may indicate your integration partner. Also, there might be a request for an in-depth exploration of your healthcare integration strategy. While not all health systems require extensive details about the process, ensuring the integration partner adheres to stringent security measures is a priority.
Fortunately, SPsoft stands out through a unique value proposition in the interoperability arena. Your sales team can leverage it to clarify the integration process and demonstrate how your product integration strategy becomes more efficient and streamlined with our support. This narrative is beneficial in discussions with health systems and when engaging investors, internal teams, or prospective partners.
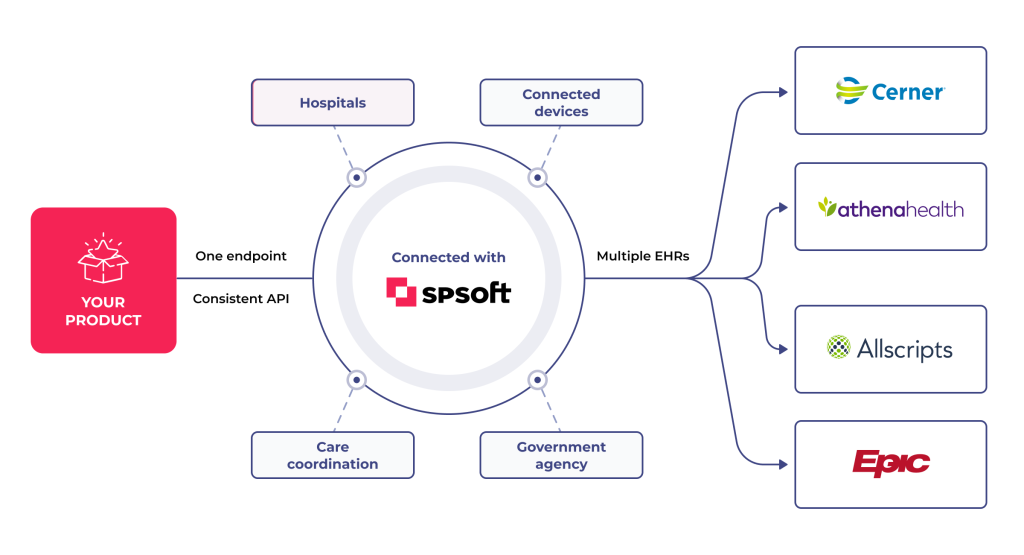
Streamlining Integration with a Modern API
SPsoft’s platform revolutionizes integration by moving away from traditional point-to-point connections. Our top-notch API offers a unified standard and connection for your application, requiring a single setup.
This approach simplifies the integration process, eliminating the need to adjust documentation delivery methods across various EHR systems like Cerner and Epic. By coding once to our platform, you bypass the need to install enterprise software or develop bespoke interfaces. That enhances scalability and efficiency as your product grows.
Navigate the future of healthcare with confidence by mastering EHR API integration. Read our informative guide to understand the ins and outs of the process!
Accelerating Growth
Your product’s integration with SPsoft brings seamless connectivity with multiple EHR systems. As you expand, our in-depth understanding of your application’s specifics allows for quicker implementation in subsequent projects. When integrating with health systems already in our network, the tech groundwork previously laid out facilitates a near-instantaneous go-live for your product. SPsoft’s platform fosters easier data exchange by optimizing current infrastructure, distinguishing it from labor-intensive point-to-point connections.
Managed Services for Hassle-Free Integration
With SPsoft, the burden of building and maintaining connections to customer EHR systems is lifted. Our comprehensive managed services eliminate the complexities of VPNs, SFTP, and other technical challenges, sparing your team from becoming network security experts. This approach simplifies connectivity and reduces the resource allocation necessary from your side.
Maximizing Health System IT Efficiency
Compared to traditional point-to-point interfaces, our healthcare integration model simplifies the workload for health system IT departments. They can save substantial time and effort without intricate message manipulation or configuration updates. On average, our project demands considerably fewer IT resources, complemented by our proactive monitoring and alerts. That ensures secure and reliable connections.
Adapting to Industry Evolutions
SPsoft’s leading API is designed to accommodate the dynamic nature of the healthcare industry, including EHR updates, system changes, or new data standards like FHIR. Our hub-and-spoke architecture and SaaS model provide the agility to make adjustments swiftly. That guarantees your application remains integrated and supported over the long term.
Choosing between a FHIR Façade and a FHIR Repository can be pivotal for your business. Discover which option aligns best with your needs in our comparison!
Positioning Your App as a Lightweight, Turnkey Solution
In an environment where health systems are approached by many applications for integration, offering a solution that demands minimal effort and maintenance from the health system makes your product highly attractive. Partnering with SPsoft positions your application as an almost immediate fit, streamlining the path to healthcare integrations and enhancing its appeal to health systems.
Thus, by choosing SPsoft, you will obtain a strategic collaboration that enhances your product’s appeal in a competitive market, promising efficiency and ease of integration to health systems.
Final Thoughts
This guide aims to equip you with a robust understanding of integration processes and relevant strategies for effectively marketing your product to health systems. By delving into it, you should possess the vital knowledge to navigate the complexities of integration, tailor your pitch to meet the specific needs of health systems and execute projects confidently. Ultimately, that will lead to successful partnerships and product implementations.
Ready to bridge the gap in healthcare interoperability? SPsoft is your partner in seamlessly integrating health systems, enhancing data fluidity, and optimizing care!
FAQ
What is healthcare system integration?
Healthcare system integration refers to connecting and coordinating various information systems within a healthcare organization or across multiple medical entities. The primary goal is to enable seamless data exchange, improved workflows, and enhanced communication.
It is about creating a unified and interconnected healthcare ecosystem where information flows freely and securely between different systems, departments, and facilities. Interconnectedness is crucial in today’s complex healthcare landscape, where patient data resides in many systems. That may include electronic health records (EHRs), practice management software (PMS), lab information systems, radiology information systems, billing systems, etc.
Healthcare system integration aims to break down these silos and create a cohesive environment where information is readily available to those who need it when they need it. That involves establishing standardized data formats, secure communication protocols, and robust integration engines to facilitate seamless data exchange between systems.
Effective integration can also support a range of advanced functionalities, such as:
– Automated data exchange. Eliminating the need for manual data entry and reducing the risk of errors.
– Real-time data access. Providing clinicians with up-to-date information at the point of care.
– Streamlined workflows. Automating appointment scheduling, billing, and claims processing tasks.
– Enhanced reporting and analytics. Enabling the generation of comprehensive reports and dashboards to track key performance indicators and identify areas for improvement.
– Improved patient engagement. Facilitating secure online access to patient records, appointment scheduling, and communication with healthcare providers.
Ultimately, health system integration is a critical enabler of value-based care, population health management, and other initiatives to improve the quality and accessibility of medical services. It is a strategic imperative for organizations seeking to thrive in such a complex environment.
What types of healthcare integrations are most common?
Several integrations are prevalent, each addressing specific needs and facilitating different aspects of data exchange and workflow optimization. Here are some of the most common:
– EHR Integration. Connecting EHRs with other clinical and administrative systems is a cornerstone of healthcare integration. That allows for the seamless exchange of patient data, including medical history, medications, allergies, lab results, and imaging reports.
– PMS Integration. Integrating PMS with EHRs streamlines administrative tasks such as appointment scheduling, billing, and claims processing. That reduces manual data entry, improves accuracy, and accelerates revenue cycle management.
– Laboratory Information System (LIS) Integration. Connecting LIS with EHRs allows for the automated transfer of lab results into patient records. That eliminates the need for manual transcription and reduces the risk of errors.
– Radiology Information System (RIS) Integration. Integrating RIS with EHRs enables the seamless exchange of imaging orders and reports, improving communication between radiologists and referring physicians.
– Picture Archiving and Communication System (PACS) Integration. Integrating PACS with EHRs allows clinicians to access and view medical images directly from patient records, facilitating more informed diagnoses and treatment decisions.
– Health Information Exchange (HIE) Integration. Connecting to a regional or national HIE allows for the secure exchange of patient data with other providers and healthcare entities, enhancing care coordination and facilitating population health management.
– Billing and Revenue Cycle Management (RCM) Integration. Integrating billing and RCM systems with EHRs and other systems streamlines the billing process, automates claims submission, and improves revenue cycle performance.
– Pharmacy Information System (PIS) Integration. Connecting PIS with EHRs allows clinicians to prescribe medication to patients seamlessly.
These are just a few examples of the many possible healthcare integrations. The types of integrations most relevant to your company depend on its size, structure, and specific needs.
What are the biggest challenges in integrating healthcare systems?
Integrating healthcare systems presents a unique set of complex challenges that require careful planning, technical expertise, and a commitment to collaboration:
– Data Standardization. One of the most significant challenges is the lack of standardized data formats and terminologies across different healthcare systems. This makes it difficult to exchange data seamlessly and accurately.
– Interoperability. Even with standardized data formats, achieving true interoperability between systems can be difficult due to system design, adoption, and security protocol variations. Ensuring they can “talk” to each other requires careful planning and testing.
– Legacy Systems. Many healthcare organizations still rely on outdated legacy systems not designed to integrate with modern technology. Upgrading or replacing these systems can be costly and time-consuming, and integrating them with newer ones is challenging.
– Data Security and Privacy. Protecting sensitive patient data is paramount. Integrating healthcare systems requires robust security measures to prevent unauthorized access, data breaches, and compliance with regulations like HIPAA and GDPR.
– Workflow Disruption. Integrating new systems can disrupt existing workflows and processes, leading to staff resistance and potential inefficiencies. Careful planning, training, and change management are essential to minimize disruption.
– Scalability and Performance. As data volumes and the number of connected systems increase, ensuring that the integrated environment can scale to meet growing demands and maintain optimal performance is crucial.
– Cost. Healthcare system integration projects can be expensive, requiring investments in software, hardware, consulting services, and staff training. Justifying the costs and demonstrating a clear return on investment (ROI) can be difficult.
– Governance and Maintenance. Maintaining an integrated healthcare environment requires ongoing governance, monitoring, and maintenance. That includes ensuring data quality, addressing security vulnerabilities, and adapting to evolving business needs.
– Lack of Technical Expertise. Integrating healthcare systems requires specialized skills in data modeling, integration techs, and workflows. Many medical organizations lack the in-house expertise to manage these projects effectively.
Successfully navigating these challenges requires a strategic approach, an expert project team, and a commitment to collaboration among all stakeholders.
Can SPsoft help integrate custom or legacy systems?
Yes, SPsoft is well-equipped to assist healthcare organizations with integrating custom or legacy systems. We recognize that many medical providers rely on a mix of modern and older systems, and we have developed expertise in bridging the gap between these environments.
Our approach to integrating both systems involves carefully assessing the current infrastructure, thoroughly understanding your needs, and creating a tailored integration strategy. We leverage various proven techniques and technologies to ensure seamless and secure data exchange between disparate systems.
Some of the key steps we take in integrating custom or legacy systems include:
– Assessment and Planning. We assess the existing systems, data formats, and workflows to identify potential integration challenges and develop a detailed project plan.
– Data Mapping and Transformation. We carefully map data elements between systems and use data transformation rules to ensure they are exchanged accurately and consistently.
– Interface Development. We develop custom interfaces and APIs to enable communication between systems that may not have built-in integration capabilities.
– Security Implementation. We implement robust security measures to protect sensitive patient data during transmission and storage and ensure compliance with regulations.
– Testing and Validation. We conduct thorough testing and validation to ensure that the integrated environment functions correctly and that data is exchanged reliably.
– Ongoing Support and Maintenance. We provide ongoing support and maintenance to guarantee the integrated environment remains stable, secure, and up-to-date.
SPsoft’s team of experienced integration specialists has a proven track record of successfully integrating custom and legacy systems for healthcare organizations of all sizes. We provide our clients with innovative, cost-effective solutions that improve data flow and patient care.
Which EHR development companies have good FHIR integration capabilities for healthcare systems?
FHIR is the modern standard for exchanging healthcare information electronically, and strong FHIR integration capabilities are crucial for building interoperable EHR systems. Several development companies specialize in leveraging FHIR for custom EHR solutions within healthcare systems. Here are five companies known for their FHIR integration expertise:
– SPsoft. SPsoft focuses heavily on modern interoperability standards, offering specialized services in FHIR integration for healthcare systems. They build SMART-on-FHIR applications compatible with major EHRs like Epic and Cerner, provide data conversion services to FHIR from legacy formats (HL7v2, CDA), develop FHIR facades to make older systems FHIR-compatible, and create custom EHR solutions leveraging FHIR for seamless, real-time data exchange.
– Smile Digital Health. Smile Digital Health is a major contributor to the FHIR standard and provides a FHIR-native clinical data platform. While they offer a core product, they also provide extensive development services and expertise around building FHIR-based solutions. Healthcare systems partner with them to implement FHIR repositories, develop FHIR APIs, and build custom applications that leverage FHIR for advanced interoperability and data management.
– Andersen. Andersen is a large custom software development company with a strong healthcare practice, offering expertise in modern interoperability standards. They provide services for implementing FHIR alongside HL7 and other standards, ensuring custom EHR solutions and integrations they build for healthcare systems facilitate seamless data exchange and meet current regulatory requirements for data sharing.
– Kanda Software. With extensive experience in healthcare software development, Kanda Software specializes in building complex, compliant solutions. They offer FHIR integration services, helping healthcare systems connect disparate applications, develop custom FHIR APIs, and ensure EHRs and related software can effectively communicate using modern interoperability standards while adhering to HIPAA and FDA regulations.
– Glorium Technologies. Glorium Technologies provides custom software development for healthcare, including EHR solutions, with a focus on interoperability and compliance. They have experience implementing FHIR standards to enable better data exchange, build custom applications that integrate with EHRs via FHIR APIs, and help healthcare systems modernize their data infrastructure for improved connectivity.
These companies offer specialized skills in FHIR implementation, API development, and data transformation, helping healthcare systems build or integrate EHR solutions that meet modern interoperability requirements.